BIOTECHNOLOGY AND MEDICAL SCIENCE
Biotechnology is a new developing field or I must say a very developed field in the field of science. It has developed many researches which have helped many faculties of science. Medicine is one of the field which it has supported for treating many diseases or if not diseases then for physiotherapy. Here below you will come across many research which biotechnology has contributed to health. Have a wonderful tour down here........
1. Decay-Fighting Microbes
Bacteria living on teeth convert sugar into lactic acid, which erodes enamel and causes tooth decay. Florida-based company ONI BioPharma has engineered a new bacterial strain, called SMaRT, that cannot produce lactic acid—plus, it releases an antibiotic that kills the natural decay-causing strain. Dentists will only need to swab SMaRT, now in clinical trials, onto teeth once to keep them healthy for a lifetime.
2. Artificial Lymph Nodes
Scientists from Japan's RIKEN Institute have developed artificial versions of lymph nodes, organs that produce immune cells for fighting infections. Though they could one day replace diseased nodes, the artificial ones may initially be used as customized immune boosters. Doctors could fill the nodes with cells specifically geared to treat certain conditions, such as cancer or HIV. I really doubt if this will work……..
3. Asthma Sensor
Asthma accounts for a quarter of all emergency room visits in the U.S., but a sensor developed at the University of Pittsburgh may finally cause that number to plummet. Inside the handheld device, a polymer-coated carbon nanotube—100,000 times thinner than a human hair—analyzes breath for minute amounts of nitric oxide, a gas that lungs produce prior to asthma attacks.
4. Cancer Spit Test
Forget biopsies—a device designed by researchers at the University of California-Los Angeles detects oral cancer from a single drop of saliva. Proteins that are associated with cancer cells react with dyes on the sensor, emitting fluorescent light that can be detected with a microscope. Engineer Chih-Ming Ho notes that the same principle could be applied to make saliva-based diagnostic tests for many diseases.
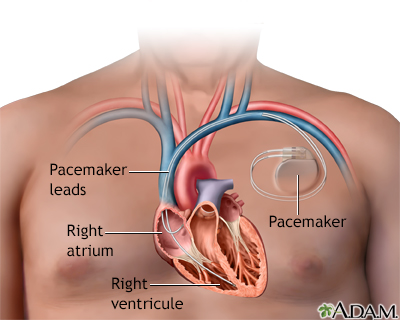
5. Biological Pacemaker
Electronic pacemakers save lives, but use hardware that eventually wears out. Now, researchers at several universities are developing a battery less alternative: pacemaker genes expressed in stem cells that are injected into damaged regions of the heart. Better suited for physical exertion, biological pacemakers have been shown to bring slow canine hearts back up to speed without complications. That’s really a good move……
6. Prosthetic Feedback
One challenge of prosthetic limbs is that they're difficult to monitor. "You and I sense where our limbs are spatially without having to look at them, whereas amputees don't," says Stanford University graduate student Karlin Bark. Skin is sensitive to being stretched—it can detect even small changes in direction and intensity—so Bark is developing a device that stretches an amputee's skin near the prosthesis in ways that provide feedback about the limb's position and movement.
7. Smart Contact Lens
Glaucoma, the second-leading cause of blindness, develops when pressure builds inside the eye and damages retinal cells. Contact lenses developed at the University of California-Davis contain conductive wires that continuously monitor pressure and fluid flow within the eyes of at-risk people. The lenses then relay information to a small device worn by the patient; the device wirelessly transmits it to a computer. This constant data flow will help doctors better understand the causes of the disease. Future lenses may also automatically dispense drugs in response to pressure changes.
8. Speech Restorer
For people who have lost the ability to talk, a new "phonetic speech engine" from Illinois-based Ambient Corporation provides an audible voice. Developed in conjunction with Texas Instruments, the Audeo uses electrodes to detect neuronal signals traveling from the brain to the vocal cords. Patients imagine slowly sounding out words; then the quarter-size device (located in a neck brace) wirelessly transmits those impulses to a computer or cellphone, which produces speech.
9. Absorbable Heart Stent
Stents open arteries that have become narrowed or blocked because of coronary artery disease. Drug-eluting stents release medication that keeps the artery from narrowing again. The bio-absorbable version made by Abbott Laboratories in Illinois goes one step further: Unlike metal stents, it does its job and disappears. After six months the stent begins to dissolve, and after two years it's completely gone, leaving behind a healthy artery.
10. Muscle Stimulator
In the time it takes for broken bones to heal, nearby muscles often atrophy from lack of use. Israeli company StimuHeal solves that problem with the MyoSpare, a battery-operated device that uses electrical stimulators—small enough to be worn underneath casts—to exercise muscles and keep them strong during recovery.
11. Nerve Regenerator
Nerve fibers can't grow along injured spinal cords because scar tissue gets in the way. A nanogel developed at Northwestern University eliminates that impediment. Injected as a liquid, the nanogel self-assembles into a scaffold of nanofibers. Peptides expressed in the fibers instruct stem cells that would normally form scar tissue to produce cells that encourage nerve development. The scaffold, meanwhile, supports the growth of new axons up and down the spinal cord.
12. Stabilizing Insoles
When Erez Lieberman's grandmother suffered a dangerous fall, he wanted to ensure it never happened again. "But it wasn't till a few years later at NASA that I found a way to channel that into something tangible," says the MIT graduate student. Using technology developed to monitor the balance of astronauts who have just returned from space, Lieberman's iShoe analyzes the pressure distribution of the feet. Doctors can use the insole to diagnose balance problems in elderly patients before falls occur.
13. Smart Pill
California-based Proteus Biomedical has engineered sensors that track medication use by recording the exact time drugs are ingested. Sand-grain-size microchips emit high-frequency electrical currents that are logged by Band-Aid-like receivers on the skin. The receivers also monitor heart rate and respiration and wirelessly transmit the data to a computer. "To really improve pharmaceuticals, we need to do what is now common in every other industry—embed digital technology into existing products and network them," says David O'Reilly, senior vice president of corporate development.
14. Autonomous Wheelchair
MIT researchers have developed an autonomous wheelchair that can take people where they ask to go. The chair learns about its environment by listening as a patient identifies locations—such as "this is my room" or "we're in the kitchen"—and builds maps using Wi-Fi, which works well indoors (unlike GPS). The current model, which is now being tested, may one day be equipped with cameras, laser rangefinders and a collision- avoidance system
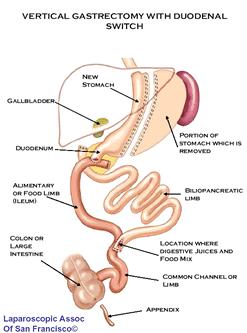
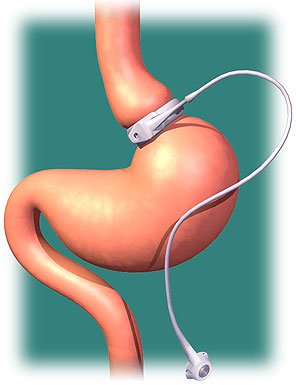
15. Gastrointestinal Liner
Obesity is associated with type II diabetes, which over time wears out the pancreas. A gastrointestinal liner developed by Massachusetts-based GI Dynamics may restore the obese to a healthy weight by preventing food from contacting the intestinal wall. The Endobarrier is routed endoscopically through the mouth—unlike a gastric bypass, no surgery is necessary—and lines the first 2 ft of the small intestine, where the most calories are absorbed (nutrients are still absorbed farther down the intestine).
16. Liver Scanner
How healthy is your liver? Until recently, answering that question often required a painful biopsy. French company EchoSens has developed a machine that scans the organ for damage in just 5 minutes. Studies have shown that damaged livers become stiffer and less elastic, so the scanner, called the Fibroscan, measures the organ's elasticity using ultrasound.
17. Nanoscale Adhesive
Gecko feet are covered with nano-size hairs that exploit intermolecular forces, allowing the lizards to stick firmly to surfaces. By replicating this nanoscale topography, MIT scientists have developed an adhesive that can seal wounds or patch a hole caused by a stomach ulcer. The adhesive is elastic, waterproof and made of material that breaks down as the injury heals.
18. Portable Dialysis
More than 15 million adult Americans suffer from diseases of the kidneys, which often impair the ability of the organs to remove toxins from the blood. Standard dialysis involves three long sessions at a hospital per week. But an artificial kidney developed by Los Angeles-based Xcorporeal can clean blood around the clock. The machine is fully automated, battery-operated, waterproof and, at less than 5 pounds, portable.
19. Walking Simulator
Stroke victims are being tricked into recovering more quickly with a virtual-reality rehabilitation program developed at the University of Portsmouth in Britain. As patients walk on a treadmill, they see moving images that fool their brains into thinking they are walking slower than they are. As a result, patients not only walk faster and farther, but experience less pain while doing so.
20. Rocket-Powered Arm
Adding strength to prosthetic limbs has typically required bulky battery packs. Vanderbilt University scientist Michael Goldfarb came up with an alternative power source: rocket propellant. Goldfarb's prosthetic arm can lift 20 pounds—three to four times more than current prosthetics—thanks to a pencil-size version of the mono-propellant rocket-motor system used to maneuver the space shuttle in orbit. Hydrogen peroxide powers the arm for 18 hours of normal activity.
THANK YOU.......